The Gulf War lasted just one year, from August 2, 1990, to July 1, 1991. Nearly 700,000 active military were deployed in Operation Desert Shield and Desert Storm. Between 30% and 40% (about 250,000) of these veterans returned home with a disabling, multisystem syndrome now called Gulf War Illness (GWI) that continues to produce pain and disability nearly 30 years later. See Box 1 for the diagnostic criteria.
| Box 1: Diagnostic Criteria for Gulf War Illness
Kansas Criteria1: Chronic symptoms in 3 or more of the following 6 domains dating to service in 1990:
Requires at least 1 moderately severe symptom or ≥ 2 symptoms in a single domain for the domain to qualify. Exclusions include: cancer, diabetes, heart disease, chronic infectious disease, liver disease, lupus, multiple sclerosis, stroke, or psychiatric condition with psychosis or requiring hospitalization since 1991. Exclusions for comorbid diseases are for research purposes. Veterans with GWI are not protected from developing these conditions, and in some cases may be at elevated risk. |
We used new methods in broad-spectrum targeted metabolomics2 in a small study of 20 veterans with Gulf War Illness3. We found that GWI was caused by a new kind of metabolic syndrome that was characterized by increased sphingolipids (ceramides and sphingomyelins) and phosphatidylcholine (PC) lipids, and decreased purines, HETEs, and endocannabinoids (anandamide and oleoylethanolamine). The specific pattern of metabolic abnormalities in GWI was distinct from ME/CFS (Figure 1). The metabolic syndrome of GWI was also found to be different from post-traumatic stress disorder (PTSD) and traumatic brain injury (TBI)3. The diagnostic pattern of lipid abnormalities in GWI was strong validation for similar findings in rat and mouse animal models of GWI that were produced by exposure to the nerve gas antidote, pyridostigmine bromide, and the insecticide permethrin4, 5.
While changes in mitochondrial function are clearly involved in pathogenesis of GWI, ME/CFS, PTSD, and TBI, the nature of the mitochondrial changes, and the specific stages of the healing cycle6 that are blocked are different in each disorder. A generalized loss of mitochondrial function does not explain the unique pattern of abnormalities observed in each of these disorders. The patterns are specific to each disease, but include some overlapping features. In GWI, the metabolic features are most consistent with persistence of cells in the proinflammatory and proliferative stages of the healing cycle—CDR1 and CDR2, respectively. In contrast, ME/CFS appears to result from a block in healing at an early stage in CDR3, with periodic crashes that retrigger the inflammatory and the pain- or autonomic and neuroendocrine dysfunction-producing aspects of CDR16.
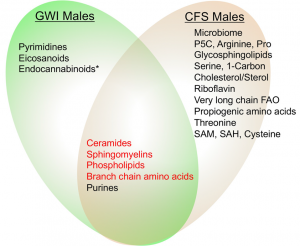 |
| Figure 1. Metabolic similarities and differences between Gulf War illness and chronic fatigue syndrome. Four of five pathways shared by males with GWI and ME/CFS were regulated in opposite directions (indicated in red). Only purines were regulated in the same direction—purine were decreased in both GWI and ME/CFS. *Endocannabinoids were decreased in females with ME/CFS, but did not reach statistical significance in males7. |
New Research
In new research funded in part by the Steven and Alexandra Cohen Foundation and private donors around the world, and supported by collaborations with Columbia University, Johns Hopkins University, and the Bay Area Lyme Foundation, we will be using advanced methods in targeted metabolomics and exposomics to answer the following questions:
- Can a combination of metabolomics and exposomics be used to improve the diagnosis of Gulf War Illness (GWI)?
- What are the differences and similarities in metabolism and the exposome between GWI, PTSD, post-treatment Lyme disease syndrome (PTLDS), and ME/CFS?
- Can a new test called “Dynamic Metabolomic Analysis” (DMA) be used to personalize metabolomic results, identify subtypes, and predict outcomes in Gulf War Illness, PTSD, Lyme, and ME/CFS?
References
- Steele L. Prevalence and patterns of Gulf War illness in Kansas veterans: association of symptoms with characteristics of person, place, and time of military service. American journal of epidemiology 2000; 152(10): 992-1002.
- Li K, Naviaux JC, Bright AT, Wang L, Naviaux RK. A robust, single-injection method for targeted, broad-spectrum plasma metabolomics. Metabolomics : Official journal of the Metabolomic Society 2017; 13(10): 122.
- Naviaux RK, Naviaux JC, Li K, Wang L, Monk J, Bright AT et al. Metabolic features of Gulf War Illness. PloS one 2019.
- Abdullah L, Evans JE, Montague H, Reed JM, Moser A, Crynen G et al. Chronic elevation of phosphocholine containing lipids in mice exposed to Gulf War agents pyridostigmine bromide and permethrin. Neurotoxicology and teratology 2013; 40: 74-84.
- Emmerich T, Zakirova Z, Klimas N, Sullivan K, Shetty AK, Evans JE et al. Phospholipid profiling of plasma from GW veterans and rodent models to identify potential biomarkers of Gulf War Illness. PloS one 2017; 12(4): e0176634.
- Naviaux RK. Metabolic features and regulation of the healing cycle-A new model for chronic disease pathogenesis and treatment. Mitochondrion 2019; 46: 278-297.
- Naviaux RK, Naviaux JC, Li K, Bright AT, Alaynick WA, Wang L et al. Metabolic features of chronic fatigue syndrome. Proceedings of the National Academy of Sciences of the United States of America 2016; 113(37): E5472-5480.